This development is good news considering that the number of donor hearts for transplants are very scarce around the world, wherein more than 25 percent of Americans who are on the national waiting list for a heart will die before receiving one. However, now there appears to be an alternative. Their study has just been published in the prestigious journal Nature Materials. The new patch, invented by Prof. Tal Dvir and doctoral student Ron Feiner of TAU’s Biotechnology Department, the Department of Materials Science and Engineering, and its Center for Nanoscience and Nanotechnology may single handedly change the field of cardiac research, they said. “With this heart patch, we have integrated electronics and living tissue,” said Dr. Dvir. “It seems like science fiction, but it’s already here, and we expect it to move cardiac research forward in a big way. Until now, we could engineer organic cardiac tissue with only mixed results. Now we have produced viable bionic tissue that ensures that heart tissue will function properly.”
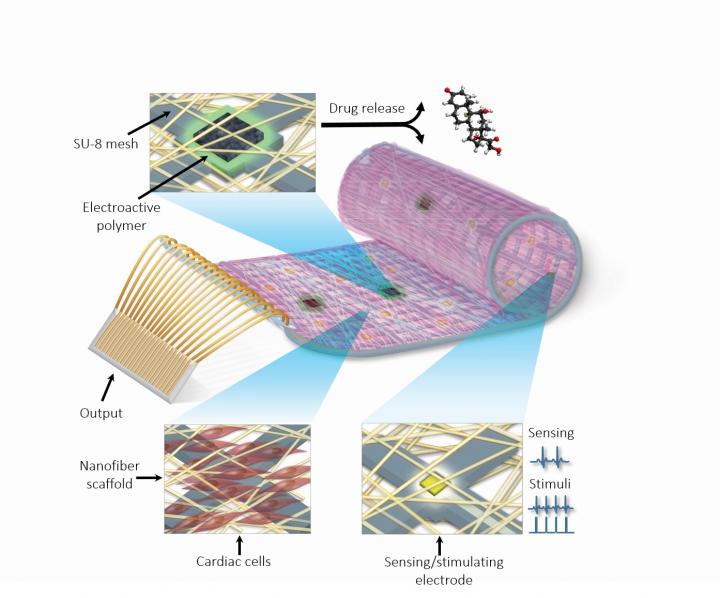
Prof. Dvir’s Tissue Engineering and Regenerative Medicine Lab at TAU has been at the forefront of cardiac research for the last five years, binding sophisticated nanotechnological tools to build functional substitutes for tissue that are damaged forever by heart attacks and cardiac disease. The new cyborg cardiac patch not only replaces organic tissue but also guarantees its sound functioning through remote monitoring. “We first ensured that the cells would contract in the patch, which explains the need for organic material,” said Dr. Dvir. “But, just as importantly, we needed to verify what was happening in the patch and regulate its function. We also wanted to be able to release drugs from the patch directly onto the heart to improve its integration with the host body.” The team has engineered thick bionic tissue suitable for transplantation for the new bionic patch. The engineered tissue features electronics that sense tissue function and as a result provide electrical stimulation. In addition, electro-active polymers are integrated with the electronics. These polymers are able to discharge medication, such as small molecules or growth factors on demand upon activation. “Imagine that a patient is just sitting at home, not feeling well,” Dr. Dvir said. “His physician will be able to log onto his computer and this patient’s file — in real time. He can view data sent remotely from sensors embedded in the engineered tissue and assess exactly how his patient is doing. He can intervene to properly pace the heart and activate drugs to regenerate tissue from afar. “The longer-term goal is for the cardiac patch to be able to regulate its own welfare. In other words, if it senses inflammation, it will release an anti-inflammatory drug. If it senses a lack of oxygen, it will release molecules that recruit blood-vessel-forming cells to the heart.” At the moment, the technology is a long way from conventional use, but the news does offer a glimpse at how bionic tissue could be used in the future. Researchers are currently examining how Dr. Dvir’s proof of concept could apply to the brain and spinal cord to treat neurological conditions. “This is a breakthrough, to be sure,” Dr. Dvir said. “But I would not suggest binging on cheeseburgers or quitting sports just yet. The practical realization of the technology may take some time. Meanwhile, a healthy lifestyle is still the best way to keep your heart healthy.”